About 9 out of 10 children, and 7 out of 10 adults with Lymphoblastic Lymphoma can be cured after their first line of treatments.
Others may need more than one line of treatment to achieve a cure or remission.
What are Lymphoblasts?
Lymphoblastic Lymphoma (LL) is a rare aggressive cancer of white blood cells called lymphoblast cells, so to understand Lymphoblastic Lymphoma, you need to know a bit about lymphoblasts.
How are lymphoblasts made?
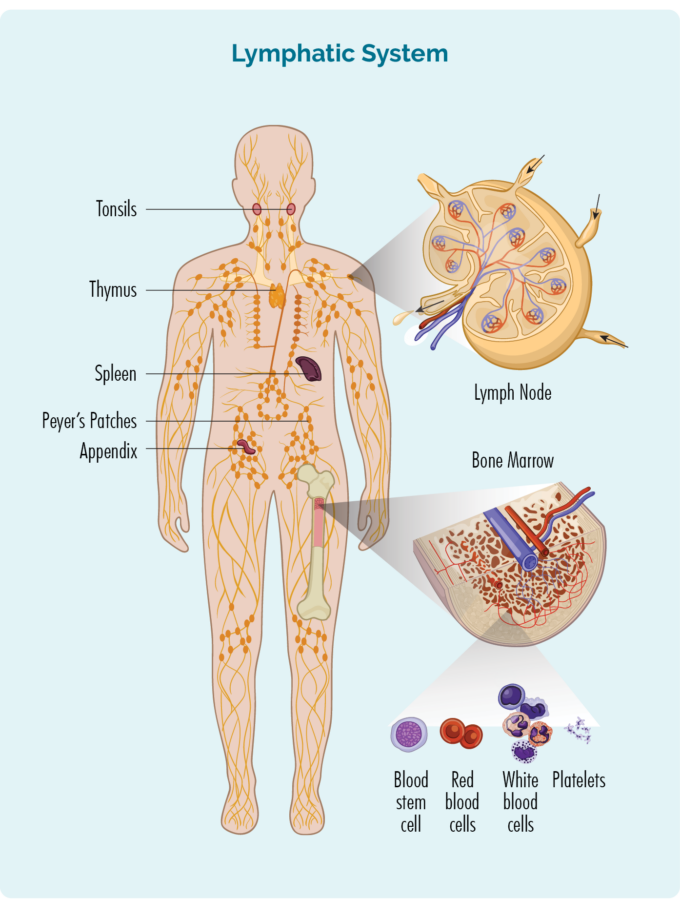
Lymphoblasts are made from stem cells in our bone marrow.
Stem cells
Stem cells are the most immature, but cleverest cells we have. They are able to get messages from different chemicals in our body and then develop into any type of cell we need.
Haematopoietic stem cells can become any type of blood cell, including red blood cells, white blood cells or platelets. These stem cells are in our bone marrow, and once they know what blood cell to become, they develop into blast cells before they mature into fully grown cells.
Haematopoietic stem cells can develop into T-cell or B-cell lymphoblast cells in our bone marrow, and then move out into our lymphatic system, thymus and spleen where they continue to develop and become mature B-cell lymphocytes, or T-cell lymphocytes.
Lymphoblasts
Lymphoblasts are a type of white blood cell in its most immature form – before it fully develops into a lymphocyte cell. Lymphocytes are an important part of our immune system that help to fight infection and disease, and also make sure our immune system does not become overactive.
Lymphoblastic Lymphoma starts when cancerous changes happen to lymphoblast cells, before they mature into lymphocytes. Because of this, you may not have enough mature lymphocytes to fight infection and disease.
Lymphocytes
Click on the headings below to learn more about B-cell and T-cell lymphocytes.
About B-Cell lymphocytes
- Are a type of white blood cell.
- Fight infection and diseases to keep us healthy.
- Memory B-cell lymphocytes remember infections we had in the past, so if we get the same infection again, our body’s immune system can fight it more effectively and quickly.
- Are made in our bone marrow (the spongy part in the middle of our bones), but usually live in our spleen and lymph nodes. Some live in our thymus and blood too.
- Can travel through our lymphatic system, to any part of our body to fight infection or disease.
- The most mature type of B-cell lymphocytes are called Plasma cells, and these cells make antibodies that are specific to each type of antigen. Antigen is a word used to describe anything that may make us sick including germs, infections, pollen or other allergens, diseased or damaged cells. Antibodies attach to the antigen to let our immune system it needs to come and fight the antigen.
About T-cell Lymphocytes
- T-cells are made in our bone marrow, mature in our thymus, but can live in any part of our lymphatic system – including our lymph nodes.
- Most T-cells need to be activated to work effectively. They are usually resting in our thymus or other parts of our lymphatic system, and only wake up and fight infection when other immune cells let them know there is an infection or disease to fight. When they wake up, T-cells can travel to any part of our body to fight the infection or disease.
- Some T-cells are responsible for “regulating” the immune response. This means that once an infection has been destroyed, the Regulatory T-cells tell other immune cells to “stand down” so they don’t keep fighting and cause harm to our good cells.
- Natural Killer (NK) cells are often called “NK T-cells”. They are specialised immune cells that recognise and destroy cancer cells. Unlike other T-cells, NK cells do not need to be activated to fight cancer. They are ready to fight at all times, and actively move around our body on the look-out for cells that have cancerous changes.
- After fighting an infection or disease, some T-cells become “Memory T-cells”. They remember everything there is to know about the infection and how to fight it. That way, if we ever get the same infection or disease again, our immune system can fight it a lot more quickly and effectively.
- Some T-cells help other immune cells, such as B-cell lymphocytes to work effectively. These T-cells are called “Helper T-cells”.
Difference between Lymphoblastic Lymphoma and Lymphoblastic leukemia
Lymphoblastic Lymphoma is very closely related to Lymphoblastic Leukemia. The table below provides a summary of the main differences between the two cancers. However, it is important to know that there is often an overlap between these two cancers. This means that you can have features of both lymphoblastic lymphoma, and lymphoblastic leukemia.
Because of this overlap, you will likely have the same treatment and outcomes whether you have the lymphoma or leukemia type.
Lymphoblastic LYMPHOMA ↓ | Lymphoblastic LEUKEMIA ↓ | |
Most commonly is cancer of | T-cell Lymphoblasts | B-cell Lymphoblasts |
Sometimes can be cancer of | B-cell Lymphoblasts | T-cell Lymphoblasts |
Cancerous cells mostly IN | Lymphatic system, skin or other organs (but can also be in bone marrow and blood) | Bone marrow and blood stream (but can also be in lymphatic system, skin or other organs) |
Symptoms of Lymphoblastic Lymphoma
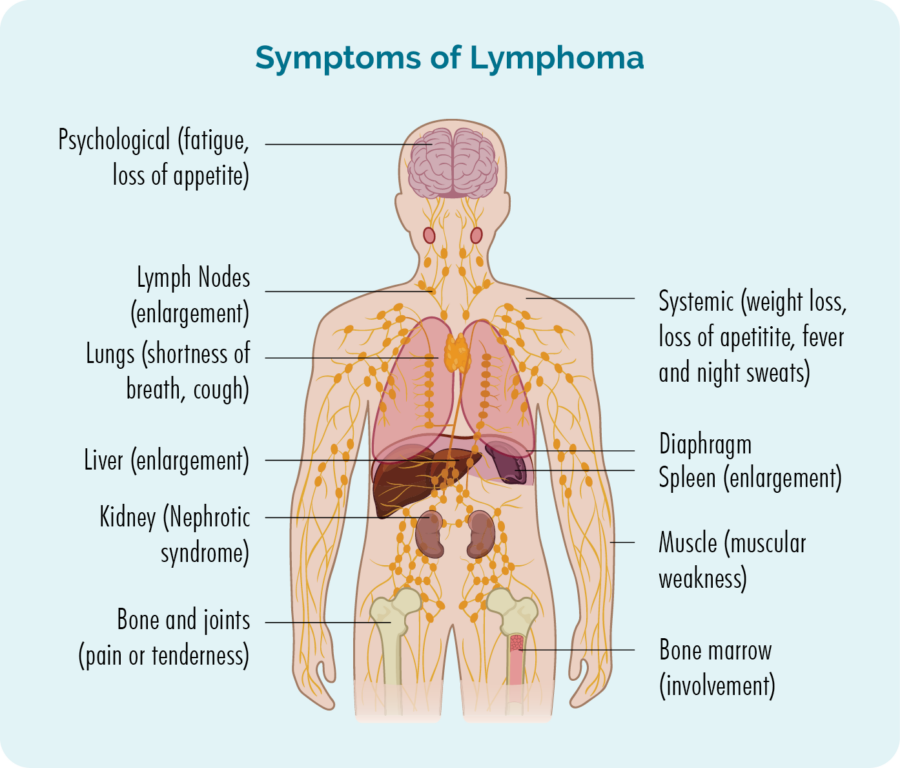
Some symptoms of Lymphoblastic Lymphoma will be similar to general symptoms anyone with any type of lymphoma can get such as:
- When you don’t have enough healthy lymphocytes, you can get lots of infections or have difficulty getting over infections.
- Too many cancerous lymphoma cells in your bone marrow can take up too much room, so your bone marrow may not be able to make other blood cells such as red blood cells, other white blood cells or platelets. A blood test may show that you have low levels of these blood cells.
- When the cancerous lymphoblasts are in your lymphatic system such as your lymph nodes or organs, they may swell up and look or feel like a lump under your skin.
- Lymphoblastic Lymphoma in your skin may give you a rash that does not go away, and may or may not be painful or itchy.
- B-symptoms – see image below.
Other symptoms
Other symptoms of Lymphoblastic Lymphoma may be specific to the area of your body the lymphoma is growing. Because lymphocytes are designed to move around our body to look for and fight and infection and disease, they can be found in any part of our body.
If the cancerous lymphocytes – the lymphoma cells gather in a part of your body you may get symptoms related to that part of your body. These symptoms are listed below. But know, you may not have any, or only get a few of these symptoms, it is unlikely you will get all of them.
- Pain that feels like it is coming from your bones.
- Swollen (or enlarged) organs such as of your liver or spleen. A swollen liver is called hepatomegaly, and a swollen spleen is called splenomegaly. When they are both swollen it is called hepatosplenomegaly.
- Hepatomegaly can cause pain in your abdomen or chest, yellowing of your skin or eyes, weight loss, pain when you drink alcohol, bruising or bleeding more than usual, or blood clots.
- Splenomegaly can cause pain in your chest or abdomen, make you feel full even when you haven’t eaten, or have eaten very little, anemia (which is low levels of haemoglobin and red blood cells), weight loss, fatigue or easy bleeding and bruising.
- Pale skin (lighter than your usual colour).
- Discomfort, pain or pressure in your chest.
- Shortness of breath or changes to how your breathing sounds.
- Changes to your voice.
- Fluid build-up in the lining around your lungs (pleural effusion, also called a PE), making it painful or difficult to breath, or around your heart (pericardial effusion) which can cause chest pain, or changes to how your heart beats.
- Superior vena cava syndrome. This is where the lymphoma starts to put pressure on your blood vessels, obstructing blood flow. You may notice veins sticking out or swelling more than usual in your chest, arms, neck and head. You may also have a cough or trouble breathing.
How is Lymphoblastic Lymphoma diagnosed?
To diagnose any type of lymphoma you will need a biopsy. There are several different types of biopsies used to diagnose lymphoma in different parts of your body. The main types of biopsies you may have if your doctor suspects you have Lymphoblastic Lymphoma include:
- Core biopsy of an affected lymph node.
- Skin biopsy of any affected skin.
- Excisional biopsy to remove an entire lymph node.
- Bone marrow biopsy to check if you have lymphoma cells in your bone marrow.
- Blood tests.
- Other biopsies of affected organs (such as thymus, liver or spleen) during surgery.
- You may also have a PET scan or CT scan to see how many areas of your body are affected.
Staging
Staging tests check to see how much of your body is affected by the lymphoma. However, even if your lymphoma is in many areas of your body, you still may be cured. The type of treatment you get, and the expected outcomes of treatments are decided by your molecular and risk stratification, rather than stage of your Lymphoblastic Lymphoma.
Molecular and Risk stratification
There are many different molecular changes that can happen on lymphoma cells, and even people with the same subtype of lymphoma can have different molecular changes. These can include:
- mutations to the genes that program your lymphocyte cells,
- different proteins and receptors that are found on the surface of your lymphoma cells.
Most people only have a few molecular changes out of hundreds of possibilities. Your haematologist is the best person to ask about your molecular and risk stratification and what it means for your individual situation.
If your lymphoma cells are positive for the Philadelphia mutation (Ph+) it means that 2 of your genes have fused together. This causes an abnormal protein to develop that helps lymphoma cells grow.
These lymphomas may respond well to a medicine called dasatinib. However, dasatinib will not work if your lymphoma does not have this mutation.
*Dasatanib is currently only available as a second line treatment, which means if your first lot of treatment does not work, or you relapse after a time of remission, and your lymphoma is Ph+, you may be able to have this treatment.
Ask your doctor
- What is my molecular and risk stratification?
- Does this impact my treatment options?
- What other treatment options and clinical trials are available for me based on this information?
- Do you expect me to be cured after treatment?
What causes Lymphoblastic Lymphoma?
We don’t know what causes most lymphomas. It is not infectious so you cannot pass it on to someone else, and it is not related to lifestyle factors such as your weight and activity levels, alcohol or smoking.
There are some things that may increase your risk of getting Lymphoblastic Lymphoma, but most people with the same risk factors never develop lymphoma, and others with none of the risk factors sometimes do get lymphoma.
Some risk factors may include if you have, or have had a:
- previous infection with Epstein-Barr virus (EBV) – this virus causes glandular fever (also called mono or the kissing disease).
- weakened immune system due to an inherited immune deficiency disease (autoimmune disease).
- infections with human immunodeficiency virus (HIV).
- immunosuppressant medication that is taken to prevent you rejecting an organ or stem cell transplant.
- if you have a brother or sister with Hodgkin Lymphoma (especially if they are your twin). However, this is a very slight increased risk and in most cases, there is no need for any genetic testing. Most people with Lymphoblastic Lymphoma have no family history.
Before treatment for Lymphoblastic Lymphoma
Multidisciplinary care
In many cases, your haematologist will meet with other haematologists and other health professionals to discuss your case. This is a great thing when you have a rare lymphoma because you get many different, very experienced people looking at your individual situation to determine the best way to help you, and make sure you get best the best treatment options and care.
You can also ask your haematologist to present your case at the Australasian Lymphoma Alliance meeting. This meeting brings together experts from around the country who are up to date with the latest research developments in rare lymphomas. They can advise your haematologist of any clinical trials or new treatment options available to you.
Whether you are male or female, many treatments can affect your fertility, making it more difficult or impossible to get pregnant, or get somebody else pregnant. If you are of child-bearing age (or younger), even if you are not thinking about having a family or extending your family just yet, you need to talk to your doctor about how to preserve your fertility, prevent unwanted pregnancies and prevent or manage early menopause or ovarian insufficiency.
When you are first diagnosed, or starting treatment after a relapse, it can be difficult to think straight and know what questions to ask. But it’s important you have all the right information you need to make the decisions about your healthcare and know what to expect. Click on the link below to download Questions to ask your doctor.
Having treatment is going to change your life and the lives of those closest to you for a while. It is important to know what to expect and prepare for. You also need to know what support is available to you. We have developed some tips on practical things you should know when you or a loved one has lymphoma. Click the link below for more information.
Starting treatment
The doctors will take into consideration many factors about the lymphoma and your general health to decide when and what treatment is best for you. They will consider:
- The subtype of Lymphoblastic Lymphoma you have.
- Whether your lymphoma is mostly in your blood and bone marrow, or lymphatic system and other parts of your body.
- Any symptoms you have.
- Your age, past medical history, physical and emotional wellbeing.
- Whether you have ever had treatment for the Lymphoblastic Lymphoma in the past.
- Your eligibility to join a clinical trial.
- Your personal preferences after you’ve been given all the information you need to make a decision.
Treatment protocols
Treatment protocols are another of way of saying what your treatment plan is. Because of the similarity between Lymphoblastic Lymphoma and Lymphoblastic Leukemia, you may have treatments similar to people with Lymphoblastic Leukemia, or other subtypes of lymphoma. This will depend on where your lymphoma is mostly growing and how it is affecting your body.
Your treatment protocol may include one or more of the following:
- Chemotherapy with or without other medicines called monoclonal antibodies such as blinatumomab.
- Stem-cell transplant.
- CAR T-cell therapy. (For B-cell Lymphoblastic Lymphoma), currently approved for under 25yr olds and expected to be approved for all B-cell Lymphoblastic Lymphoma patients in the near future.
- Clinical trial.
If you have very early-stage disease and the lymphoma is not in your blood or bone marrow, you may have radiation or surgery, though this would be rare.
Does age matter?
- Younger patients may only need chemotherapy to be cured (but may or may not also have a stem cell transplant).
- Middle aged people may be offered less intensive chemotherapy and a stem cell transplant to be cured.
- Older people may have treatment to control their disease and put into remission rather than be cured.
Induction, consolidation and maintenance
Your chemotherapy protocol may include an induction, consolidation and/or maintenance phase to get you into, and keep you in remission or to increase your chance of cure.
Induction treatments usually last several months however, maintenance treatment can continue for about 2 years.
Finishing treatment
Finishing treatment can be exciting, or a very anxious time for you. It could even make you feel both excited and anxious.
It is normal to feel many different emotions when you finish treatment. And, even if you coped well during treatment, you may find that once everything slows down and you have time to think about what you’ve been through, and how to get back to some kind of life that resembles life before treatment, you become overwhelmed.
You also have to deal with the emotions of others around you and their expectations. Many patients mention how hard it is when people around them expect them to be back to normal long before they are ready.
On the other hand, other patients have mentioned feeling like people around them hold on too tight and don’t let them get back to normal, because they are afraid something else might happen.
We have tips on what to expect, and how to manage emotions, and the expectations of other on our Finishing treatment webpage.

Follow up
You will continue to see your haematologist or oncologist regularly even after treatment ends. They will assess you for any ongoing side-effects from treatment, or any new side-effects that can happen months or even years after treatment ends. You can find more information about late effects by clicking the side effects of treatment link above.
They will also be assessing you signs for any signs of your lymphoma relapsing so that any needed treatment can start as soon as possible.
Your follow-up appointments may include any of the below:
- PET or CT scans and results.
- Blood tests.
- Physical examination of your lymph nodes.
- Questions about how you are feeling, and adapting to life after treatment.
- Referrals for extra care if needed.
Summary
- Lymphoblastic Lymphoma is the 2nd most common subtype of lymphoma in children.
- Anyone can develop Lymphoblastic Lymphoma including older adults, but it is more common in children and young adults about 30 years of age.
- There are two main subtypes including B-cell Lymphoblastic Lymphoma and T-cell Lymphoblastic Lymphoma.
- Lymphoblastic Lymphoma is an aggressive lymphoma needing treatment soon after diagnosis. However, most people will be cured after their first line of treatment.
- Symptoms may be related to general symptoms of lymphoma, or specific to the area of your body the lymphoma is growing. Report all new and worsening symptoms to your doctor.
- Ask if you are eligible to join a clinical trial if you are newly diagnosed with Lymphoblastic Lymphoma, or it relapses after and time of remission.
- Finishing treatment is exciting, but can come with challenges. Make sure you visit our Finishing treatment page to find out what to expect and how to prepare for life after treatment.